CDC works closely with state and local governments, people with and at risk for HIV, as well as federal partners to coordinate efforts on expanding the use of the highest-impact HIV prevention strategies: Diagnose; Treat; Prevent; and Respond. As needed, CDC will assist each jurisdiction to address gaps in their local workforce.
While the specifics of implementation will differ by jurisdiction and funding, each community will be working to scale up four key strategies which together can end the epidemic:
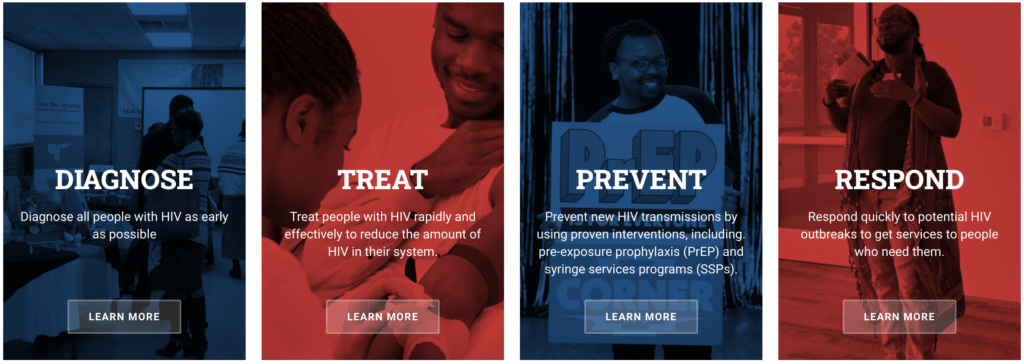
DIAGNOSE
Diagnose all people with HIV as early as possible
Great strides have been in made in HIV prevention, but about 1 in 7 (14%) of the estimated more than 1 million people with HIV in America still don’t know they have HIV.
In 2006, CDC recommended that all people ages 13 to 64 be tested for HIV at least once in healthcare settings. However, uptake of that recommendation has not been optimal.
CDC will work in collaboration with communities and other agencies to increase local capacity to expand HIV testing according to CDC guidelines, so that all people with HIV in the high-burden areas receive a diagnosis. Key approaches will include:
- Using the latest systems and technology to make HIV testing simple, accessible, and truly routine in healthcare and non-healthcare settings.
- Carrying out focused approaches that encourage more people who are at substantial risk for HIV to get tested for HIV at least annually.
- Ongoing collaboration to identify and implement innovative technologies and programs, such as self-testing, to make testing more accessible.
- Working with funded recipients to adapt plans to meet the HIV prevention needs of their communities and address current service challenges and disruptions due to COVID-19. Examples of approaches could include:
- use or expansion of telemedicine and telehealth
- rapid HIV self-tests or mail-in self-tests
- other locally tailored creative solutions
TREAT
Treat people with HIV rapidly and effectively to reach sustained viral suppression
Current HIV treatment guidelines recommend all people with HIV begin treatment as soon as possible after receiving a diagnosis. Local community plans will be pivotal to expanding HIV treatment and care services to all people with HIV, especially to populations disproportionately affected by HIV.
People who have HIV and who take medication daily as prescribed and maintain an undetectable viral load, can live long, healthy lives and have effectively no risk of sexually transmitting the virus to an HIV-negative partner. About 80% of HIV infections that occur each year are transmitted by people who are not receiving HIV care. As part of its role in Ending the HIV Epidemic, CDC will:
- Collaborate with partners and providers, so that people who receive a positive test result for HIV are quickly linked to care and HIV treatment started as soon as possible after diagnosis. Healthcare provider training and education resources on HIV care and treatment from the Health Resources and Services Administration (HRSA) will be available in the identified communities where CDC will be expanding HIV testing. In addition, HRSA-supported community health centers and Ryan White HIV/AIDS Program centers in these communities are being funded to provide healthcare and support services for people with newly diagnosed HIV.
- Help partners expand local programs that identify and follow up with people who have stopped receiving HIV care and treatment. Data-to-Care tools and approaches will encourage them to get back in HIV care and treatment.
PREVENT
Prevent new HIV transmissions by using proven interventions, including pre-exposure prophylaxis (PrEP) and syringe services programs (SSPs)
The HIV epidemic affects communities differently. Locally designed plans will guide the scale-up proven interventions, such as PrEP and SSPs, to address communities’ unique needs.
PrEP
PrEP is a pill that reduces the risk of getting HIV when taken as prescribed. Fewer than 25%
of the estimated more than 1 million Americans who could benefit from PrEP are using this prevention medication. As part of Ending the HIV Epidemic, state and local communities, in partnership with CDC and other federal agencies, will implement strategies to increase access to and use of PrEP—especially among African American and Latino gay and bisexual men, African American women, and other populations disproportionately affected by HIV.
As part of its role in Ending the HIV Epidemic, CDC:
- And the Health Resources and Services Administration (HRSA) will train healthcare providers on prescribing and managing PrEP, and HRSA will work to increase the availability of PrEP services in community health centers.
- And the Substance Abuse and Mental Health Services Administration (SAMHSA) will conduct outreach to people at highest risk so they know PrEP is available and how to access it.
- Will continue to update clinical guidelines for prescribing PrEP, and add more public and private providers who offer PrEP to its PrEP Locator.
- Will continue to provide education campaigns for both the public and healthcare providers to combat stigma associated with PrEP use, as well as the stigma associated with HIV.
Comprehensive SSPs
Comprehensive SSPs have been shown to dramatically reduce HIV risk and can provide an entry point for a range of services to help stop drug use, overdose deaths, and infectious diseases. Research shows that new users of SSPs are five times more likely to enter drug treatment, and about three times more likely to stop using drugs than people who don’t use the programs.
Yet many communities now threatened by the opioid epidemic and increasing injection drug use have not had the resources to establish effective SSPs. CDC will work with SAMHSA to increase access to and use of comprehensive SSPs, and will work with local communities to implement SSPs where they are needed and permitted by state and local laws.
CDC issued guidance on how to deliver these critical HIV prevention services during disruptions in clinical services. This includes offering guidance for providing PrEP when facility-based services and in-person patient-clinician contact is limited, as well as interim guidance for SSP programs operating during the COVID-19 pandemic.
RESPOND
Respond quickly to potential HIV outbreaks to get needed prevention and treatment services to people who need them
Cutting-edge HIV prevention technologies and strategies now allow CDC to help local public health officials identify where HIV prevention and treatment services are most urgently needed.
Real-time response systems are key to ending the HIV epidemic in the United States. While CDC has been working to increase response capacity nationwide, not all areas have the resources to identify, investigate, and respond to potential HIV outbreaks.
CDC will assess and address gaps in staffing, expertise, and data management systems that prevent states and local areas from being able to fully investigate and respond to increases in HIV transmission and outbreaks — and to take HIV prevention and treatment resources to where they are needed quickly.
